Past Issues
Case Report of Opioid Free Anesthesia Combined with Errector Spinae Plane Block for Lumbar Spinal Fusion Surgery
Leonids Solovjovs1,2, Artis Gulbis3,4, Janis Nemme3,5, Aleksejs Miscuks4, Inara Logina2, Jelena Dukate3, Agnese Ozolina1,2*
1Clinic of Anaesthesiology, Riga East University Hospital, Hipokrata street 2, LV 1038, Riga, Latvia
2Riga Stradinš University, Dzirciema street 16, LV 1007, Riga, Latvia
3Orto Clinic, Bukultu street 1a, LV 1005, Riga, Latvia
4University of Latvia, Faculty of Medicine, Raina Bulvaris 19, LV 1586, Riga, Latvia
5Department of Anaesthesiology and Intensive Care, Pauls Stradins Clinical University hospital, Pilsonu street 13, LV 1002, Riga, Latvia
*Corresponding author: Agnese Ozolina, Clinic of Anaesthesiology, Riga East University Hospital, Hipokrata street 2, LV 1038, Riga, Latvia, Tel: +371-265-541-85; E-mail: [email protected] Received: September 28, 2020 Published: October 23, 2020
ABSTRACT
A novel regional anesthesia technique when local anesthetic is injected into the fascial plane between the transverse process of the vertebra and the erector spinae muscles has been demonstrated in lumbar spinal surgery patients with controversial results. Here, we report a case of an 83 year old female, physical status class (ASA) II class, with moderate depression and chronic back pain scheduled for transpedicular fusion surgery at 4 to 5 lumbar level and lumbar laminectomy. We performed opioid free anesthesia with ketamine in combination with bilateral single-shot Erector Spinae Plane Block (ESPB) at fourth lumbar level providing the loss of sensation bilaterally from Thoracic 11 to Sacral 2. This allowed to dismiss the need for intraoperative opioids as well as secured stable hemodynamics during surgery. In postoperative period patient was pain-free with block lasting up to 24 hours and minor opioid consumption. Patient experienced only mild pain, no strong severe pain, 2-3 points in Numeric Rating Scale (NRS), before discharge on 9th postoperative day. Moderate depression with a score of 13 out of 27 points was recorded during the pre-operative assessment with Patient Health Questionnaire-9 (PHQ-9), this score decreased to 4 points out of 27 at discharge. Disability level presented as Oswestry Disability index (ODI) improved from 30/50 or 60% to 10/50 or 20% at discharge.
Opioid free anesthesia with ketamine in combination with single-shot bilateral ESPB at the lumbar level for lumbar spine fusion surgery proved to be an effective and safe method in terms of analgesia, activation, level of depression and disability.
KEYWORDS: Opioid free anesthesia, Erector spinae plane block, Spinal fusion, Numerological pain score
INTRODUCTION
While opioids are first-line agents for postoperative pain, those are associated with significant adverse effects, including tolerance and induced hyperalgesia as well as systemic reactions and potentially abuse, particularly for chronic back pain patients. It is well known, that opioid anesthesia does not reduce postoperative pain, which is the main reason for unwilling activization, significantly affecting recovery [1]. A novel regional anesthesia technique when local anesthetic is injected into the fascial plane situated between the transverse process of the vertebra and the erector spinae muscles is defined as Errector Spinae Plane Block (ESPB). The local anesthetic is assumed to penetrate the superior costotransverse ligament and reach the paravertebral space providing analgetic effect [2,3]. The first time ESPB has been demonstrated successfully whilst treating thoracic neuropathic pain and postoperative pain in thoracic surgery in 2016 by Forero M, et al. [4].
Recently, ESPB increasingly has been used in lumbar spine surgery patients due to its effect on dorsal ramus of spinal nerve which gives the sensory innervation to components of dorsal column of spine providing painless back area after spinal surgery [3]. However, in a systematic review published by Qiu Y, et al. [5], was concluded the effectiveness and safety of this block is still controversial in lumbar spine surgery.
We hypothesized, that ketamine instead of phentanyl in combination with ESPB might reduce the rates of opioid consumption and their associated side effects during and after surgery as well as to have a positive effect on incidence of chronic pain, levels of depression and disability. The aim of this case report is to demonstrate effectiveness and safety of ESPB in combination with opioid free anesthesia for lumbar spinal fusion surgery. This case highlights the benefit of this approach on postoperative pain level, levels of depression and disability following spine surgery.
CASE REPORT
An 83-year-old female was admitted for transpedicular fusionsurgery and laminectomy at lumbar 4-5 level.Magnetic resonance imaging (MRI) revealed a lumbo-sacral spondylolisthesis and L4-L5 stenosis as seen in figure 1.
Figure 1: Magnetic resonance image in lateral position.
The patient's medical history included dyslipidemia, well controlled hypertension, type 2 diabetes, and total hysterectomy seven years ago due to uterine cancer. The patient was over weight (weight 82 kg, height 1.68 m, body mass index 29.1 kg/m2). She complained of a chronic (>3 months) back pain in lumbar region, which did not respond to paracetamol, non-steroidal anti-inflammatory drugs, opioids (Codeine, Tramadol), physical therapy. Signs of moderate depression were observed. The patient was diagnosed with physical status class (ASA) II. Patient had 5 effective facet joint blocks which released pain, however following the sixth block which was not effective patient agreed to undergo a surgical treatment.
A preoperative neurological examination showed motor impairment in right lower limb without sensory deficits. She did not present hyperalgesia or allodynia. Pain was located in the lumbar area with irradiation to right gluteal area. Pain severity was rated by numerological pain score (NRS) before the surgery and registered as NRS of 8 when moving and NRS of 5 when resting. Paravertebral palpation was painful on the right side at L4-L5 levels.
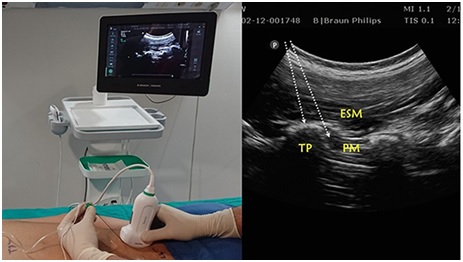
After the induction of general anesthesia with midazolam (Dormicum® 5mg/ml, F.hoffmann-La Roche Ltd., Switzerland), 2.5 mg, ketamine (Calypsol® 50mg/ml, Gedeon Richter LTD, Hungary), 2 mg/kg, propofol (Propofol® 10mg/ml, Fresenius Kabi AG, Germany), 2 mg/kg, cisatracurium (Nimbex®, 2mg/ml, Aspen Pharma Ltd, Ireland) 0.2 mkg/kg the patient was intubated and placed in the prone position. Bilateral ultrasound guided ESPB at the lumbar level L4 was then performed. A high-frequency linear ultrasound transducer was placed in a parasagittal orientation 3 cm lateral to the L4 spinous process.
At this level the only muscle identified superficial to the hyperdense transverse process is the erector spinae muscle (Figure 2).
Figure 2: (A) Position and orientation of the ultrasound transducer during a parasagittal scan of the lumbar region with the subject in the prone position. (B) Ultrasound images of Tulgar approach for lumbar erector spinae plane block. White arrow indicates needle with in-plane approach. Abbreviations: TP: Transverse Process; ESM: Erector Spinae Muscle; PM: Psoas Muscle. Reprinted from Tulgar S, et al. [6].
A 50 mm 22 G ultrasoundneedle (BRAUN®, Germany) was inserted in-plane in a cephalad to caudal direction until bone contact with the top of the transverse process. After slight retraction of the needle, 20 ml of 0.25% Bupivacaine (Bupivacaine-Grindex, 5 mg/ml, Grindex, Latvia) with 100 mcg (1:200.000) Epinephrin (Adrenaline, 1mg/ml, Sopharma Ad. Bulgaria) as an adjuvant was injected deep to the erector spinae muscle and cephalad to caudal spread of the local anesthetic was promptly observed. The same procedure was repeated on the contralateral side. During the surgery standard monitoring was performed according to American Society of Anesthesiology standards [7].
Anesthesia was maintained with Sevoflurane (Sevorane®, AbbVie S.r.l., Italy) and with intravenous Ketamine (Calypsol® 50mg/ml, Gedeon Richter LTD, Hungary) in infusion 0.5 mg/kg/h. The patient remained hemodynamically stable throughout the procedure. Mean arterial pressures were maintained at around 70 mmHg and heart rate around 70-90 beats per minute, with no need for vasopressors or hypotensive agentsor additional opioids. The two levels (L4-L5) transpedicular fusion surgery and lumbar laminectomy (Figure 3) lasted for 2 hours 15 min in the prone position, after which the patient was placed supine and uneventfully extubated in 15 minutes after the end of surgery. The patient awoke absolutely pain-free (NRS 0-1) and without nausea. She presented slightly confused in the first 20 minutes after the surgery but was able to communicate properly and convincingly controlling her airways.
Figure 3: X-ray image in and in anterior-posterior (a) and lateral (a) position on the second postoperative day after onelevel L4/5 fusion surgery and laminectomy.
Postoperatively, hemodynamic monitoring was followed regularly; fluid management and oxygen supply were provided in the intensive care ward for first 24 hours. The patient was assessed for pain control 1, 8, 12 and 24 hours after the surgery.
An immediate postoperative neurologic assessment revealed no motor impairment of the lower extremities but an extensive sensory block to both Pinprick test and a cold were detected. On the back, the sensory loss extended bilaterally from Th 11 to S2, buton the front, up to Th 9 on the left and Th 10 on the right from S3. This evaluation was performed every 12 hours after the surgery and remained unchanged until 24 hours after surgery, when the sensory block finally receded.
During the first 24 postoperative hours, the patient had received multimodal analgesia with Acetaminophen (Paracetamol, B. Braun Melsungen AG, Germany) 1 g IV every 6 hours and Dexketoprofenum (Dolmen®, 25 mg/ml, Berlin-Chemie/Menarini, Germany) 50 mg IV every 12 hours. Patient Controlled Analgesia IV pump with fentanyl was offered as an option when needed. The pump had no baseline infusion, but was allowed a bolus of 20 mcg of fentanyl every 10 min. In the first 24 hours after surgery, patient not required any fentanyl. On the second day, the pump was removed. According to hospital guidelines multimodal analgesia orally was provided with Dexketoprofenum (Dolmen®, Berlin-Chemie/Menarini, Germany) 50 mg every 12 hours, Acetaminophen (Paracetamol, B. Braun Melsungen AG, Germany) 1g every 6 hours, pregabalin (Lyrica®, Pfizer, USA) 150mg every 24 hours. For pain exacerbation if NRS >5, combination of Dexketoprofenum/Tramadol (Skudexa®, Menarini – Von Heyden GmbH, Germany) 75/25 mg were given. Postoperative thrombosis prevention was provided with enoxaparin 40 mg (Clexane®, Sanofi-Aventis S.A. Spain) once daily from the first postoperative day.
The postoperative period was uneventful. She remained pain-free at rest, and the maximum reported pain score on movement was mild (NRS 3–4 out of 10). The most severe pain was observed in the evening before bedtime with NRS 5 to 6. During hospital stay (10 days total stay, 8 postoperative days) she received 7 doses of Dexketoprofenum/Tramadol. Patient was discharged on the ninth postoperative day pain-free with no neurological symptoms. The patient also noticed improved mood, better appetite and improved sleep after surgery.
The effect on early postoperative period in terms of incidence of chronic pain, level of depression Patient Health Questionnaire-9(PHQ-9)and Oswestry Disability index (ODI) was observed [8,9]. Preoperative assessment showed moderate depression (PHQ-9, 13 points of 27) and severe disability (ODI 30/50 or 60%). At discharge patient showed improved scores, her depression and disability level were minimal (PHQ-9, 4 points of 27 and ODI 10/50 or 20%).
DISCUSSION
Standard opioid anesthesia with patient-controlled analgesia is still widely used after a major spinal fusion surgery. Moreover, epidural injection analgesia is applied in some clinics also. In addition, perioperative opioid use in patients undergoing spine surgery is linked to increased length of stay as well as to worse outcomes as demonstrated by decreased ODI [10,11]. On the other side there is an increasing number of publications, that demonstrate the beneficial effect on post-operative morphine consumption and improvement of postoperative well-being after the opioid free anesthesia [1,12,13]. Ketamine – NMDE receptor antagonist with newly found neuroprotective, anti-inflammatory, anti-tumorous and antidepressant properties might show the positive long-term effect in terms of mental health and sleeping disorders, particularly, in chronic back pain patients with signs of depression [14].
ESPB is an interfacial plane block where a local anesthetic is injected in a plane preferably below the erector spinae muscle. It has been demonstrated as an effective and safe regional analgesic technique, with numerous applications in thoracic, breast, abdominal, spinal and even orthopedic surgeries, particularly when compared to paravertebral block and epidural analgesia due their well-known risks and side effects [4,5,15]. ESPB is supposed to work at the origin of spinal nerves spreading cranio-caudally for up to 7 dermatomal levels depending on local anesthetic volume [15]. Wide spreading of local anesthetic was confirmed also in our case report providing sensory block up to 4 levels and down to 3 levels from lumbar level 4 where the bilateral injection was performed with 20 ml of 0.25 % Bupivacaine combined with 100 mcg Epinephrine. Singh found that injection of 0.5%-20 ml Bupivacaine bilaterally at the Th8 level last for 6-8 hours after surgery [16]. Epinephrine as an adjuvant might prolong the block [15]. Despite the fact, that vasoactive agent additive to long acting local anesthetic doesn’t improve block for longer than one hour, we used 100 mcg of Epinephrin or 2.5 mcg per one ml of local anesthetic when performing this block as suggested by other authors [15,17]. In our presented patient ESPB provided effective postoperative analgesic affect for 24 hours. Also, Dexamethasone 2 ml (8 mg) has been applied as an adjuvant in combination with long-lasting local anesthetic and provided effective analgesia for 24 hours after anterior approach thoracolumbar surgery [18]. The safe and most effective dose and concentration of local anesthetic for ESPB are still unknown. Most of case studies report single-shot bilateral injection of long-lasting local anesthetic (Bupivacaine 0.5% or 0.25%, Ropivacaine 0.2%-0.375%) a total of 40 ml in thoracic level (Th 6,8,12), only few researchers performed ESPB in lumbar region (L1-4) with a total of 30-40 ml long-lasting local anesthetic [5,19,16]. In our case we assume that larger volume or concentration of local anesthetic unlikely would prolong the duration of block.
Besides, opioid free anesthesia with Ketamine allowed to avoid opioid administration during the operation and to reduce its requirement in postoperative period, therefore we did not observe any opioid caused side effect. Perioperative analgesia with sub-anesthetic Ketamine dose is effective and safe for acute pain in variety of contexts. American Society of Anaesthesiologist also stated that ketamine can be used as a stand-alone drug or adjunct to opioids in postoperative analgesia plan [20].
In postoperative period the patient had low pain score (NRS 2-3) when moving and no pain when resting and was able to move independently once her rehabilitation period started on the second day. The patient noted better mood, had good sleep and appetite, her depression and disability levels reduced from 13 to 4 points of 27 (PHQ-9) and ODI from 30/50 or 60% reduced to 10/50 or 20%. This allowed faster recovery and discharge. The last-mentioned effects on depression and disability might be explained by Ketamine wide effects on NMDA receptors. Not to mention ketamine’s anesthetic, analgesic, bronchodilation effects, nowadays are also widely discussed its anti-depression effect as published by Berman RM, et al. [19].
Among peripheral blocks, ESPB is a relatively new block, and there are quite a few studies in its application in lumbar spine surgery, and it will be important to conduct further studies with a larger sample to replicate our results [4]. This finding is confirmed in systematic review published by Zhen Hua and co-authors [5] where the analgetic effect of ESPB was controversial based on an analysis of four case reports, four case studies, one retrospective cohort study and two randomized controlled trials, including 171 participants. Importantly, that conclusion was mainly based on case series, one more time certifying that more randomized controlled studies in this field are needed.
Based on this case report, opioid free anesthesia with Ketamine combined with ESP block may be considered as an option or adjunct for pain management in this very particular group of patients.
CONCLUSION
Opioid free anesthesia with Ketamin supplemented with ESPB seems to be safe enough, innovative strategy that ensures good postoperative analgesia following the lumbar spine surgery and contributes to a faster patient recovery, reduced opioid requirement, improved levels of depression and disability and an earlier activation. We further aim to increase the number of participating patients to increase the significance of demonstrated results.
ACKNOWLEDGMENTS
All authors have contributed equally drafting or revising the manuscript. We thank Orto Clinic, the major Orthopedic and Vertebral Surgery private center in Riga, Latvia, for kind collaboration.
CONFLICT OF INTEREST
There are no existing financial interests or any conflict of interest regarding this manuscript.
REFERENCES
- Frauenknecht J, Kirkham KR, Jacot-Guillarmod A, Albrecht E. (2019). Analgesic impact of intra-operative opioids vs. opioid-free anaesthesia: a systematic review and meta-analysis. Anaesthesia. 74(5):651–662.
- Onishi E, Toda N, Kameyama Y, Yamauchi M. (2019). Comparison of Clinical Efficacy and Anatomical Investigation between Retrolaminar Block and Erector Spinae Plane Block. BioMed research international. 2019:2578396.
- Kot P, Rodriguez P, Granell M, Cano B, Rovira L, Morales J, et al. (2019). The erector spinae plane block: a narrative review. Korean journal of anesthesiology. 72(3):209–220.
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. (2016). The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Regional anesthesia and pain medicine. 41(5):621–627.
- Qiu Y, Zhang TJ, Hua Z. (2020). Erector Spinae Plane Block for Lumbar Spinal Surgery: A Systematic Review. Journal of pain research. 13:1611–1619.
- Tulgar S, Ahiskalioglu A, DeCassai A, Gurkan Y. (2019). Efficacy of bilateral erector spinae plane block in the management of pain: current insights. Journal of pain research. 12:2597–2613.
- Standards for Basic Anesthetic Monitoring, American society of Anesthesiologists. Available from: www.asahq.org. Accessed on: October 28, 2015.
- Kroenke K, Spitzer RL, Williams JB. (2001). The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine. 16(9):606–613.
- Fairbank JC, Pynsent PB. (2000). The Oswestry Disability Index. Spine. 25(22):2940–2952.
- Naik BI, Nemergut EC, Kazemi A, Fernández L, Cederholm SK, et al. (2016). The Effect of Dexmedetomidine on Postoperative Opioid Consumption and Pain After Major Spine Surgery. Anesthesia and analgesia. 122(5):1646–1653.
- Gessler F, Mutlak H, Tizi K, Senft C, Setzer M, et al. (2016). Postoperative patient-controlled epidural analgesia in patients with spondylodiscitis and posterior spinal fusion surgery. Journal of neurosurgery. Spine. 24(6):965–970.
- Bello M, Oger S, Bedon-Carte S, Vielstadte C, Leo F, et al. (2019). Effect of opioid-free anaesthesia on postoperative epidural ropivacaine requirement after thoracic surgery: A retrospective unmatched case-control study. Anaesthesia, critical care & pain medicine. 38(5):499–505.
- Hontoir S, Saxena S, Gatto P, Khalife M, Ben Aziz AM, et al. (2016). Opioid-free anesthesia: what about patient comfort? A prospective, randomized, controlled trial. Acta anaesthesiologica Belgica. 67(4):183–190.
- Hudetz JA, Patterson KM, Iqbal Z, Gandhi SD, Byrne AJ, et al. (2009). Ketamine attenuates delirium after cardiac surgery with cardiopulmonary bypass. Journal of cardiothoracic and vascular anesthesia. 23(5):651- 657.
- Kirksey MA, Haskins SC, Cheng J, Liu SS. (2015). Local Anesthetic Peripheral Nerve Block Adjuvants for Prolongation of Analgesia: A Systematic Qualitative Review. PloS one. 10(9):e0137312.
- Singh S, Choudhary NK, Lalin D, Verma VK. (2019). Bilateral ultrasound-guided erector spinae plane block for postoperative analgesia in lumbar spine surgery: a randomized control trial. J Neurosurg Anesthesiology. 32(4):330-334.
- Neal JM. (2003). Effects of epinephrine in local anesthetics on the central and peripheral nervous systems: Neurotoxicity and neural blood flow. Regional anesthesia and pain medicine. 28(2):124-134.
- Calandese F, Adduci A. (2019). Errector spinae block for acute postoperative pain management after anterior thoraco lumbar spine surgery. J Clin Anesthesia. 52:55-56.
- Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, et al. (2000). Antidepressant effects of ketamine in depressed patients. Biological psychiatry. 47(4):351–354.
- Schwenk ES, Viscusi ER, Buvanendran A, Hurley RW, Wasan AD, et al. (2018). Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Acute Pain Management From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Regional anesthesia and pain medicine. 43(5):456–466.
Copyright: Ozolina A, et al. ©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Ozolina A. (2020). Case Report of Opioid Free AnesthesiaCombined with Errector Spinae Plane Block for Lumbar Spinal Fusion Surgery. Surgeries. 2(1):06.
 Abstract
Abstract  PDF
PDF