Past Issues
Endometrial Follicular B Lymphoma
Julia Manzanares López1, María Sánchez Villalobos2, Elena Gurrea Almela1, Joaquín Gómez Espuch2, María del Pilar Marín Sánchez1*, Isabel Ñiguez Sevilla1
¹Department of Obstetrics and Gynaecology, Hospital Universitario Virgen de la Arrixaca, Murcia, Spain 2Department of Hematology, Hospital Universitario Virgen de la Arrixaca, Murcia, Spain
*Corresponding author: María del Pilar Marín Sánchez, Department of Obstetrics and Gynaecology, Hospital Universitario Virgen de la Arrixaca, Murcia, Spain.
Received: October 12, 2019 Published: November 13, 2019
ABSTRACT
Primary lymphomas of the female genital tract (PLFGT) are extremely rare. It’s more frequent that they appear as a dissemination of the disease. The ovaries are the most common site of PLFGT, followed by the cervix, whereas lymphoma of the endometrium is extremely rare. We present a case of a 61 year-old woman with follicular endometrial B lymphoma, a Non-Hodgkin’s lymphoma. In spite of it being rare, we must include it in the differential diagnosis along with other gynecological cancers and it’s important to know how to manage it. Biopsy and immunohistochemistry are essential for diagnosis and the treatment is chemotherapy R-CHOP.
Keywords: Non-Hodgkin’s lymphoma (NHL); Primary Lymphoma of the Female Genital Tract (PLFGT); Endometrium; Inmunohistochemistry; R-CHOP.
INTRODUCTION
Primary non-Hodgkin’s lymphoma (NHL) is a malignant monoclonal proliferation of lymphoid cells that affects the lymph nodes (nodal). It also may arise from lymphatic cells located in solid organs (extranodal) and it accounts for 25 to 35% of all NHL. Most of the sites related to this disease are in the gastrointestinal tract and the central nervous system. Primary lymphoma on the female genital tract (PLFGT) is a rare disease, which comprises 0.2 to 1.1% of all extranodal lymphomas in the female population [1,2].
CASE REPORT
61-year-old postmenopausal woman who consults a gynecologist for spotting and weight loss. Her medical history shows diabetes mellitus type II being treated with oral antidiabetics. She was appendectomized at age 14. As for the gynecological background she has an obstetric formula G3P2A1 and presented menopause at 53 years. Follow-up in breast consultations due to a BIRADS III nodule. A gynecological ultrasound (Figure 1) was performed showing edematous
myometrium and atrophic endometrium. A hysteroscopy with biopsy was indicated, which reported low-grade small cell follicular lymphoma B. In the immunohistochemical study the cells were PAX-5 (+), as well as C20, CD10 and CD79a positive. They also expressed BCL-2 (Figure 2).
Figure 1: Gynecological ultrasound of uterus. A, B and C) Longitudinal section of the uterus showing edematous myometrium and atrophic endometrium. D) 3D reconstruction of uterus.
Figure 2: Endometrial biopsy. Histopathology and immunohistochemistry. A) HE 10x, Image showing hemorrhage and a dense lymphoid aggregate, superficial fragments of endometrial glands are observed. B) HE 40X, Cellular detail, where small lymphocytes are observed, some with cleft forms (centrocytes). C) HE 40X, Endometrial glands within a lymphoid aggregate composed of small lymphocytes, some cleft, with low-grade nuclear characteristics. D) 20x, BCL-2 positive. E) 20x, BCL-6 positive. F) 20x, CD20 positive, immunohistochemical positivity of lymphocytes with CD20, strain marker B.
Tumoral markers were negatives and LDH levels were normal. A bone marrow aspiration and biopsy results did not show malignant cells in the cytometry or cytology. A thoracoabdomino- pelvic CT was performed where there were no axillary adenopathies. Adenopathies were observed in the retrocava, pretracheal, precarinal, subcarinal and in the right pulmonary hilum. Small retroperitoneal adenopathies below the renal arteries were also found. No pelvic or inguinal adenopathies were appreciated.
PET-CT showed adenopathic conglomerate in mediastinum occupying inferior paratracheal space, aortopulmonary window and subcarinal region with extension to the right pulmonary hilium reaching SUVmax value of 13.4. A diffuse metabolic increase in the uterine cavity of 2.3 cm × 3.1 cm could also be seen, which reached SUVmax value of 10.1. The diagnosis was, therefore, a low-grade follicular lymphoma stage IVA. FLIPI 1. The case was presented in a multidisciplinary Tumor Committee deciding treatment with six cycles chemotherapy R-CHOP (rituximab, cyclophosphamide, hydroxydaunorubicin, vincristine and prednisone/prednisolone) and maintenance treatment with Rituximab bimothly for two years (twelve cycles). Treatment which the patient is currently undergoing. The patient is in periodic follow-up by hematology and gynecology for physical examination and blood counts, including LDH. She has not presented side effects from the chemotherapy. PETCT for restaging after 3 cycle and after completion of firstline chemotherapy were normal, as were the gynecological ultrasounds. At the present time, the patient is in complete remission.
DISCUSSION
Lymphomas are malignant tumors that affect the immune system, most commonly the lymph nodes. Primary extranodal lymphomas account for 20% to 34% of all cases of NHL [3]. Lymphomas are classified according to a system established by the World Health Organization (WHO). The WHO classification distinguishes lymphoid neoplasms derived from precursor lymphoid cells from those derived from mature lymphoid cells and further separates each group into neoplasms of Bcell or T-cell origin. For the most part, mature lymphoid neoplasms comprise the non-Hodgkin lymphomas (NHLs); Hodgkin lymphomas are considered separately [4]. The NHL account for 90% of all malignant lymphomas and is the seventh most common malignancy and the eighth most common cause of cancer death [5]. The incidence of NHL, especially extranodal lymphoma, has increased in recent decades. The etiology of this increase could be due to infectious agents such as HIV and other viruses, immunosuppressive therapies, environmental exposures and improved diagnostic techniques, although the etiology of most types of NHL remains elusive [3].
In contrast to Hodgkin lymphoma, extranodal involvement is more frequent in non-Hodgkin lymphoma as well as dissemination to noncontiguous nodes with involvement of different nodal groups. Extranodal lymphomas are commonly subdivided as primary (primary origin in the organ) and secondary (secondary involvement of the organ) although these designations can become ambiguous and arbitrary [3]. Primary lymphoma refers to the following: 1) lymphomatous involvement confined to a solitary extranodal site and its immediately adjacent lymph node group or contiguous structures at the time of diagnosis; 2) the absence of abnormal cells in the peripheral blood and bone marrow; and 3) the absence of further lymphomatous lesions at remote sites after several months [6].
The main histological subtypes of nonHodgkin’s lymphoma are the diffuse large Bcell lymphoma, follicular lymphoma, and Burkitt lymphoma. It usually occurs in women during the fifthdecade of life. Nevertheless, it depends on the histological subtype; as an example, diffuse large B-cell lymphoma is more common between 35 and 45 years old, whereas follicular lymphoma is more frequent in people aged over 50 [2].
Primary lymphoma on the female genital tract (PLFGT)
When the female genital tract is compromised, which represents 30% to 40% of the cases [7], it is usually secondary to disseminated disease. Primary lymphoma involving the female genital tract is an uncommon condition (less than 1%). The ovaries are the most common site of PLFGT, followed by the cervix, whereas lymphoma of the endometrium is extremely rare [2,6].
However, Kosari and Daneshbod [8] found that of 186 cases of lymphomas in the female genital tract, total of 117 cases (63%) were classified as primary lymphomas of the female genital tract and 69 cases (37%) as secondary lymphomas. The most frequent lymphoma was Diffuse large B-cell lymphoma followed by follicular lymphoma and the adnexa the most frequent organ. No significant age difference was detected between primary and secondary lymphomas.
The etiology of primary B-cell lymphoma of the endometrium is unknown. Lymphocytes are a significant population of the normal human endometrium and may also be arranged as nodular aggregates [1]. However, chronic inflammation, frequently with lymph follicle formation, has been associated with several types of extranodal B-cell lymphoma. The endometrial lymphoid tissue is a regionally specialized component of the immune system that plays a role in local immune surveillance, implantation, immunosuppression, cytokine-induced placental development in early pregnancy and regulation of endometrial epithelial proliferation [9].
The diagnosis is very difficult because of the rarity of this entity. The symptoms include vaginal bleeding, vaginal discharge, an abdominal mass, dispareunia, perineal discomfort, urinary retention, or constitutional symptoms [6] and it can look like a gynecological tumor. The “B” symptoms are not frequent in this population, unless the disease has an aggressive behavior along with a large tumor burden. In the follicular lymphoma subtype, the clinical presentation usually has an indolent course [2] and the survival rate is very high.
The diagnosis is always histopathological with determination of the specific cell type by immunohistochemical study. The follicular differentiation of a lymphoma is given by the expression of CD20, BCL2 and CD10. Having the marker Ki67+ indicates high proliferative index [10]. Imaging plays important role in the non-invasive management of including the establishment of a provisional staging of disease, and follow-up. Ultrasonography (US) can be useful in the initial investigation of primary lymphomas the female genital tract, but computed tomography (CT) magnetic resonance imaging (MRI) are better for the lesion size, structure and extension to adjacent structures. PET-CT is valuable for the identification of disease in organs, the differentiation of posttreatment fibrosis residual viable tumor, detection of early recurrence, of an early response to chemotherapy, and determination prognosis [6].
NHL can sometimes be associated with abnormal CA 125 levels (7) Elevated CA-125 (concentrations above 35 U/ml) at the time of diagnosis of NHL has been associated with a decreased 5-year survival rate. Higher levels of CA-125 were associated with advanced disease stage, extranodal disease, bulky tumors, occurrence of B symptoms, pleural and peritoneal effusions, involvement of bone marrow, high serum LDH levels, high serum beta2 microglobulin and poor performance and response to treatment [5].
Primary endometrial disease may appear as diffuse thickening of the endometrium without myometrial involvement or as a polypoid lesion with or without a diffuse coating of the endometrium. Endometrial hyperplasia, endometrial polyps, and carcinoma can have similar morphologic aspects and must be considered in the differential diagnosis [6].
The prognosis usually is analyzed based on the Ann Arbor staging system (Table 1) [7,11] size and extension of the disease, age, number of node saffected, LDH level, and lymphoma’s grade [2].
Table 1: Ann Arbor staging system [11].
|
I |
Involvement of a single lymph-node region or lymphoid structure |
|
II |
Involvement of two or more lymph-node regions on the same site of the diaphragm |
|
III |
Involvement of lymph-node regions on both sides of the diaphragm |
|
IV |
Disseminated (multifocal) involvement of one or more extranodal organs or tissues, with or without associated lymph-node involvement or isolated extralymphatic organ involvement with distant (non-regional) nodal involvement |
|
A or B |
A: No symptoms; B: Fever (temperature > 38ºC), drenching night sweats, unexplained loss of more than 10% of body weight during the previous 6 months |
|
E |
Involvement of an extranodal site that is contiguous or proximal to the known nodal site |
The International Prognostic Index (IPI) is a prognostic tool that was originally developed in patients with clinically aggressive non-Hodgkin lymphoma (e.g., diffuse large B cell lymphoma) and uses patient age, serum lactate dehydrogenase, performance status, stage, and number of extranodal disease sites to predict overall survival rates. In follycular lymphoma, the main prognostic indexes that have been used are the FLIPI 1 and FLIPI 2, that include [12]:
FLIPI 1:
• Age >60 years • Stage III or IV • Hemoglobin level <12.0 g/Dl • Number of involved nodal areas >4 • Serum lactate dehydrogenase level greater than the upper limit of normal
FLIPI 2:
• Age >60 years • Hemoglobin level <12.0 g/Dl • Bone Marrow involvement • Maximal diameter of lymph node > 6 cm • Increased β2-microglobulin
Regarding the treatment, the patients who present with limited-stage disease can be treated with radiotherapy or rituximab in monoterapy, altough usually therapy is deferred symptomatic patients with advanced disease o “large tumoral mass” at diagnosis can be treated with R-CHOP Alternative treatments in patient with cardiac disease are CVP (cyclophosphamide, vincristine, and prednisone) or Rbendamustine. Maintenance treatment with Rituximab every 2 months for 2 years in patients with folicular lymphoma who have obtained complete or partial remission after induction has been shown to prolong disease-free survival. Cyclophosphamide is considered a high risk gonadotoxic drug and vincristine a medium risk.
The prognosis of uterine lymphoma is considered to be relatively favorable when the disease is in early stage and treated properly [1,5], being best assigned using the IPI, which is a powerful predictor of outcome in all subtypes of non- Hodgkin’s lymphoma [9].
CONCLUSION
Follicular endometrial lymphoma is a very rare entity. Due to the nonspecific clinic that it produces, it is easy to confuseit with other gynecological pathologies. For this reason, it is important to rule it out as a possible diagnosis. Biopsy and immunohistochemistry being essential for such task. R-CHOP is the treatment of choice for this type of lymphomas. Due to the small number of cases there is no established action protocol.
REFERENCES
- Thomas GJ, Dogan A (2004) Primitive BG. Primary low-grade B-cell lymphoma of the endometrium. Histopathology 45(6): 654-656.
- Miura LY, Maure MAD, Zomer MT, Ribeiro R, Cavalcanti TCS, Kondo W (2018) A Case of Primary Uterina Lymphoma Presenting with Bleeding, Pelvic Pain, and Dysmenorrhea. Case Rep Obstet Gynecol 2018: 5065738, 1-4.
- Silva V, Correia P, Oliveira N, Sa L (2015) Primary vaginal non- Hodgkin’s Case Report lymphoma: report of a rare clinical entity. Clin Pract 5(4): 821.
- Jiang M, Bennani NN, Feldman AL (2017) Lymphoma classification update: T-cell lymphomas, Hodgkin lymphomas, and histiocytic/dendritic cell neoplasms. Expert Rev Hematol 10(3): 239-249.
- Vijayakumar S, Serur E, Bybordi B, Lakhi N (2016) Gynecologic Oncology Reports Primary gynecological non-Hodgkin’s lymphoma: A differential diagnosis of a pelvic mass. Gynecol Oncol Rep 18: 29-31.
- Vieira MAA, Cunha TM (2014) Primary lymphomas of the female genital tract: Imaging findings. Diagn Interv Radiol 20(2): 110-115.
- Bhagat N, Kalkur P, Kalkur (2019) Primary non-Hodgkin’s lymphoma of the vagina ( PNHLV ): a gynaecologist‘s enigma! BMJ Case Rep 12(5): e228544.
- Kosari F, Daneshbod Y, Krams M, Wacker H,Parwaresch R (2005) Lymphomas of the female genital tract: a study of 186 cases and review of the literature. Am J Surg Pathol 29(11): 1512-1520.
- S. Lemos, E. Magalhaes, V. Sousa, M. Dias, C de Oliveira (2008) Primary endometrial B-cell lymphoma: case report. Eur J Gynaecol Oncol 29(6): 656-658.
- Ferrando M, Marcos C, Carmona V, Nohales F (2010) Gynecologic presentation of pelvis lymphoma. Clin Invest Ginecol Obstet 37(2): 75-78.
- Matasar MJ, Zelenetz AD (2008) Overview of Lymphoma Diagnosis and Management. Radiol Clin N Am 46(2): 175- 198.
- Arnold S Freedman, MDJon C (2019) Clinical manifestations, pathologic features, diagnosis, and prognosis of follicular lymphoma. [Internet].
Citation: Marín Sánchez MDP (2019). Endometrial Follicular B Lymphoma. Surgeries 1(1): 5.
Copyright: Marín Sánchez MDP, et al. ©2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
 Abstract
Abstract  PDF
PDF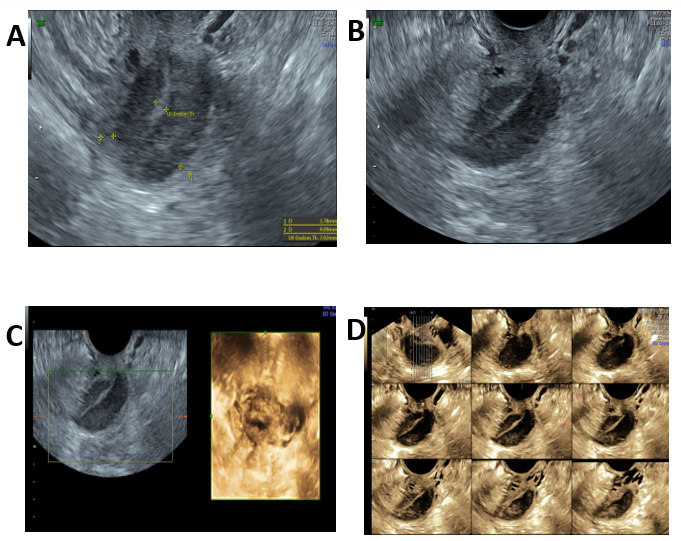
.bmp)