Past Issues
Laparoscopic Management of Postventriculoperitoneal Shunt Abdominal Pseudocyst in 10 Years Old Girl
K Karavdic1*, A Karamustafic1, N Herenda2
¹Clinic for Paediatric Surgery, Clinical University Centre in Sarajevo, Bosnia and Herzegovina 2Clinic for Anaesthesia and Reanimation, Clinical University Centre in Sarajevo, Bosnia and Herzegovina
*Corresponding author: Kenan Karavdic, Department of Pediatric Surgery, Clinical Center of University Sarajevo, Patriotske lige 81, 71000 Sarajevo, Bosnia and Herzegovina.
Received: September 23, 2019 Published: October 30, 2019
ABSTRACT Ventriculoperitoneal shunt VPS well established procedure in the treatment of pediatric hydrocefalusa can be encumbered with many complications of which is one of the rarest of the formation abdominal pseudocyst (AP).
The pseudocyst wall is covered with inflammatory fibrotic tissue, unlike true cysts whose wall is covered with mesothelium. Treatment of abdominal pseudocysts involves resection of the pseudocyst wall and shunt replacement. The above procedure can be done by open or minimal access to the surgical procedure. A 10-year-old girl to whom the VPS is placed comes from long-term abdominal colic and symptoms similar to an acute abdomen. We treated the girl with minimal access to the procedure, performed a resection from the abdominal pseudocyst, and did a VPS replacement. The patient’s postoperative course was satisfactory.
Keywords: Hydrocephalus; Pseudocyst; Laparoscopy; Shunt; Pediatric
INTRODUCTION
Hydrocephalus in the pediatric age usually leads to increased intracranial pressure. A common surgical procedure presented by a neurosurgeon is placement of a ventriculoperitoneal shunt. Parietal peritoneum cavity is the most acceptable area for receiving ventricular fluid due to low complication rate. After the first ventriculoperitoneostomy, which was done in 1905, these operations became most applicable in the treatment of congenital hydrocephalus [1,2].
VPS problems related to the abdominal can result in infections, disconnection, perforation, penetration or obstruction of hollow viscera, catheter extrusion, volvolus, hernias and intrabdominal pseudocysts. The walls of pseudocysts are not composed of mesothelium, but of fibrous tissue or inflamed serosal surface. Pressure in the pseudocyst space may increase which may interferes with VPS function.
In case of complications, the clinical picture depends on the worsening of the condition in the neurological and gastrointestinal tract. Symptoms can include vomiting, bloating, obstruction, abdominal pain, fever, palpable mass, headache [3,4]. Treatment is usually pseudocyst excision and shunt replacement.
CASE REPORT
Patient was 10 years old girl, with VP shunt from birth. The girl had a third degree intraventricular hemorrhage by birth with consecutive development of hypertensive hydrocephalus. A ventriculoperitoneal shunt was immediately performed after diagnosis.
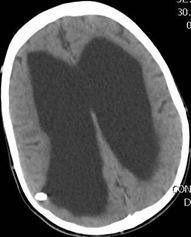
She has been having abdominal pain characterized by spasms for a month before admission to our Clinic.The symptoms were intensified 15 days before coming to our Clinic when the girl was crying because of constant abdominal pain. She was hospitalized at a regional hospital for intense abdominal pain. She did not have fever, did not vomit, had no problems with urination. She had a stool every second or third day with the help of teas. Her mother gave her occasional analgesics due to intense abdominal pain. She refused the meals, abdominal pain intensifies during the night when crying become more intense. She had a fever to 38 oC. Radiological examinations were performed and a CT scan of the brain showed an enlarged ventricular system, initial development from hydrocephalus, with a VP shunt placed in the area of the right ventricle with the apex traced at the border of the ventricles and brain parenchyma.
Due to the intensification of the problems and the suspicion of an acute surgical condition, the patient is transferred from the regional center to our Pediatric Surgery Clinic.
On admission, patients with general poor condition, dormant, respond to painful stimuli, subcutaneous adipose tissue reduced, abdomen diffusely painful to palpation. A nasogastric probe is obtained, to which a brown liquid content is obtained. During the physical examination, the abdomen was diffusely painfully sensitive. Laboratory tests are performed CRP = 196, ECHO shows a lot of free thick fluid, an abdominal RTG is performed which shows top of ventriculoperitoneal catheter subhepatically (Figure 1, 2).
Figure 1, 2: RTG shows the end of the VP shunt subhepatically.
Ultrasound has shown changes in the appearance of intestinal curvatures that are edematous are observed irregularly, pockets of denser fluid content with some significant reaction of the surrounding mesentery, and significant mesenteric adenopathy in this region are occasionally observed.
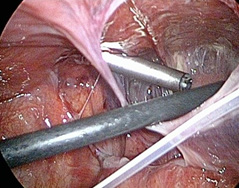
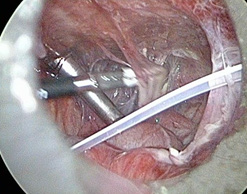
Due to suspected acute surgical disease, emergency surgery is initiated after preoperative preparation. During laparascopic surgery, pneumoperitoneum and placement of the first umbilical trocar is performed with an open Hasson procedure. It was difficult to insert other trocar because of the increments. Pseudocyst formations in the cavum recto-uterine Douglas and right pararectally are noticeable. All the while the VP shunt is attached to the small intestines by the tight attachments, (Figure 3, 4).
Figure 3, 4: VP shunt is attached to the small intestines by the tight attachments.
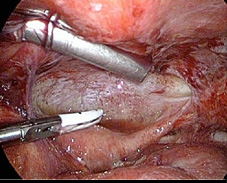
Removing the walls of the pseudocyst liberated the abdominal cavity and removes the adhesions between the intestinal loops (Figure 5, 6, 7).
Figure 5, 6: Removing the walls of the pseudocyst with blunt grasper and removes the adhesions between the intestinal loops between each other and between the intestinal loop and the anterior abdominal wall.
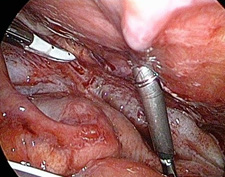
It was performed almost complete resection of the pseudocyst and complete liberalization and release of cavum recto-uterine Douglasi. (Figure 7, 8, 9, 10) There is a lot of blurry content between the adherents and the walls of the pseudocyst.
Figure 7, 8: Near total cyst excision and adhesiolysis.
The top of the ventriculoperitoneal catheter was in the subhepatic space between the margo inferior of liver, gallbladder, and intestinal loops. (Figure 11) The tip of VP shunt was released and noted to be functional and drain clear cerebrospinal fluid. The walls of the pseudocyst formation located subhepatically are not liberalized because they are very firm and due to the possibility of injury to the gallbladder, liver parenchyma and small intestine. The tip of the VP shunt is replaced to the Douglasi recto uterine cavum (Figure 12).Drainage were performed
Figure 9, 10: Complete liberalization and release of cavum recto-uterine Douglasi.
Figure 11, 12: The tip of VP shunt placed in subhepateclly pseudocyst formation and replaced in cavum recto-uterina Douglasi.
CT postoperatively was without changes in comparation with preoperative (enlarged ventricular system, initial development from hydrocephalus, with a VP shunt placed in the area of the right ventricle with the apex traced at the border of the ventricles and brain parenchyma) (Figure 13).
Figure 13: Control CT - enlarged ventricular system, initial development from hydrocephalus, with a VP shunt placed in the area of the right ventricle with the apex traced at the border of the ventricles and brain parenchyma.
Ophthalmologist fundus finding is normal. The neurosurgeon recommends the treatment of a competent neurosurgeon in regional hospital.
The postoperative course is satisfactory. The patient was placed in the Intensive Care Unit. Antibiotic therapy is administered postoperatively: Metronidasol, Meropenem and Vakomycin. She was controlled by a neurosurgeon and an ophthalmologist.
The general condition is satisfactory, the patient has no pain, the peristalsis is established, the patient does not fever, the threads are removed and the patient is transferred to a regional medical center for further outpatient treatment.
Figure 14: Appearance of anterior abdominal wall after laparoscopy treatment of abdominal pseudocyst patient.
DISCUSSION
Harsch was the first to use an abdominal pseudocyst as a medical term in 1954 [5]. In 1955, Jackson and Snodgrass also described abdominal pseudocyst (APC) in their publications. The degree of this complication in the surgical procedure for placement of VPS in congenital hydrocephalus is about 4.5%. The most likely cause of this complication is a reaction from the parietal peritoneum to the foreign body and an increased amount of cerebrospinal fluid (20 ml/h) to be absorbed [7]. This all events can lead to the challenge of the epithelium of the peritoneum, creating adhesions and the creation of the collection of cerebrospinal fluid [7,8]. Also, infection can be the cause of this disease and it is always necessary to take a sample for microbiological analysis [9].
Symptomatology can be from the neurological tract as well as from the gastrointestinal tract. Neurological symptoms that are more pronounced in the pediatric age may be related to an increase in intracranial pressure: headache, vomiting, and disorder of consciousness. Gastrointestinal symptoms are more pronounced in adult patients and may be accompanied by abdominal pain, abdominal distension, tenderness, signs of ileus, and mass in abdomen, like our patient, 10 years old girl. If there are signs of pseudocyst inflammation, the patient may have fever.
There are no clear guidelines to treating an abdominal pseudocyst today. Paracentesis has been described as one of the methods in the treatment of APV [7,8,9]. Recently lysis of adhesions and pseudocysts with laparoscopic-assisted surgery were used [10]. Recommended treatment of non-infected APC is minimal access surgery with excision of pseudocyst wall and replacement of the tip of the ventriculoperitoneal catheter. An open surgical approach with extensive resection of a pseudocyst wall may disrupt future resorption of cerebrospinal fluid and hinder future eventual placement of AV shunt. VP shunt complications were treated with the peritoneoscopy method for the first time by Morgan in 1979 [11,12,13]. The procedure we have presented in this case report was first published by Kim et al. in 1995, where they described their experience with a 12 year old boy [14]. They resected part of the APC, like in our case report, and moved the tip of the catheter to another part of the peritoneal space. Brunori et al. have published their experiences with patients with APC. They laparoscopically punctured APC space and evacuated cerebrospinal fluid [15]. Jain et al. presented 2 adult APC patients treated with minimal surgery access [16]. They were able to solve the pseudocyst and to keep VP shunt in peritoneal cavity. Esposito and the authors have recommended a minimal surgery approach to treatment of APC as safe and with a low complication rate [17]. APC treatment should be performed with 3 trocar 5 millimeter diameter with precision work, lysis of adhesion and pseudocyst wall removal. It is necessary to check the catheter tip and see if the catheter is functional and replace the catheter tip in place with maximum possibility of absorption, Douglas space [18,19]. The biggest advantage of minimal access surgery is the possibility of entering into all parts of the abdomen, lysis of adhesion and the possibility of replacing the tip of the catheter.
CONCLUSION
The advantages of minimal access surgery in the treatment of the abdominal pseudocyst are a better approach to the abdominal cavity, the ability to remove all attachments, and the ability to better position the tip of the catheter.
REFERENCES
- Guice KS, Kosloske AM (1978) Recurrent pseudocyst from a ventriculoperitoneal shunt. An unusual abdominal mass. Am J Dis Child 132(3): 285-286.
- Rainov N, Schobess A, Heidecke V, Burkert W (1994) Abdominal CSF pseudocysts in patients with ventriculo-peritoneal shunts. Report offourteen cases and review of the literature. Acta Neurochir (Wien) 127(1- 2): 73-78.
- Egelhoff J, Babcock DS, McLaurin R (1985) Cerebrospinal fluid pseudocysts:Sonographic appearance and clinical management. Pediatr Neurosci 12(2): 80-86.
- Goldfine SL, Turetz F, Beck AR, Eiger M (1978) Cerebrospinal fluid intraperitoneal cyst: An unusual abdominal mass. AJR Am J Roentgenol 130(3): 568-569.
- Harsch GR (1954) Peritoneal shunt for hydrocephalus, Utilizing the fimbria of the fallopian tube for entrance to the peritoneal cavity. J Neurosurg 11(3): 284-294.
- Jackson IJ, Snodgrass SR (1955) Peritoneal shunts in the treatment of hydrocephalus and increasedintracranial pressure. A 4-year survey of 62 patients. J Neurosurg 12(3): 216-222.
- White B, Kropp K, Rayport M (1991) Abdominal cerebrospinal fluid pseudocyst: Occurrence after intraperitoneal urological surgery in children with ventriculoperitoneal shunts. J Urol 146(2): 583-587.
- Gutierrez FA, Raimondi AJ (1976) Peritoneal cysts: A complication of ventriculoperitoneal shunts. Surgery 79(02): 188-192.
- Parry SW, Schuhmacher JF, Llewellyn RC (1975) Abdominal pseudocysts and ascites formation after ventriculoperitoneal shunt procedures. Report of four cases. J Neurosurg 43(4): 476-480.
- Holcomb GW 3rd, Smith HP (1995) Laparoscopic and thoracoscopic assistance with CSF shunts in children. J Pediatr Surg 30(12): 1642-1643.
- Morgan WW (1979) The use of peritoneoscopy in the diagnosis and treatment of complications of ventriculoperitoneal shunts in children. J Pediatr Surg 14(2): 180-181.
- Armbruster C, Blauensteiner J, Ammerer HP, Kriwanek S (1993) Laparoscopically assisted implantation of ventriculoperitoneal shunts. J Laparoendosc Surg 3(2): 191-192.
- Basauri L, Selman JM, Lizana C (1993) Peritoneal catheter insertion using laparoscopic guidance. Pediatr Neurosurg 19(2): 109-110.
- Kim HB, Raghavendran K, Kleinhaus S (1995) Management of an abdominal cerebrospinal fluid pseudocyst using laparoscopic techniques. Surg Laparosc Endosc 5(2): 151-154.
- Brunori A, Massari A, Mascarone-Palmieri R, Benini B, Chiappetta F (1998) Minimally invasive treatment of giant pseudocyst complicating ventriculoperitoneal shunt. Minim Invasive Neurosurg 41(1): 38-39.
- Jain S, Bhandarkar D, Shah R, Vengsarkar U (2003) Laparoscopic management of complicated ventriculoperitoneal shunts. Neurol India 51(2): 269-270.
- Esposito C, Porreca A, Gangemi M, Garipoli V, De Pasquale M (1998) The use of laparoscopy in the diagnosis and treatment of abdominal complications of ventriculoperitoneal shunts in children. Pediatr Surg Int 13(5- 6):352-354.
- Mobley LW 3rd, Doran SE, Hellbusch LC (2005) Abdominal pseudocyst: predisposing factors and treatment algorithm. Pediatr Neurosurg 41(2): 77-83.
- Popa F, Grigorean VT, Onose G, Popescu M, Strambu V, Sandu AM (2009) Laparoscopic treatment of abdominal complications following ventriculoperitoneal shunt. J Med Life 2(4): 426-436.
- Pinto FC, de Oliveira MF (2014) Laparoscopy for ventriculoperitoneal shunt implantation and revision surgery. World J Gastrointest Endosc 6(9): 415-418.
- Hamid R, Baba AA, Bhat NA, Mufti G, Mir YA, Sajad W (2017) Post ventriculoperitoneal shunt abdominal pseudocyst: challenges posed in management. Asian J Neurosurg 12(1): 13-16.
- Salomao JF, Leibinger RD (1999) Abdominal pseudocysts complicating CSF shunting in infants and children. Report of 18 cases. Pediatr Neurosurg 31(5): 274-278.
Copyright: Karavdic K, et al. ©2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Karavdic K (2019). Laparoscopic Management of Postventriculoperitoneal Shunt Abdominal Pseudocyst in 10 Years Old Girl. Surgeries 1(1): 3.
 Abstract
Abstract  PDF
PDF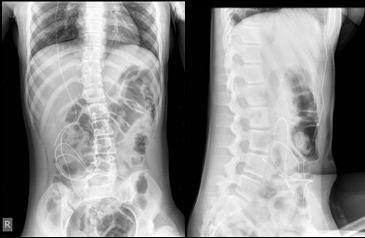
.bmp)
.bmp)
.bmp)