Past Issues
Post Laparoscopic Myomectomy Gossypiboma with Cecum and Appendix Invasion: Case Report
Hossein Negahban1, Neda Karkeabadi2, Mehrdad jor gholami3, Seyed morteza Bagheri4, Saeid Esmaeilian5*
1General Surgeon, Deylam Hospital, Bushehr University of Medical Sciences, Deylam, Iran
2General Surgeon, Tehran University of Medical Sciences, Tehran, Iran
3General Radiologist, Bushehr University of Medical Sciences, Deylam, Iran
4Department of Radiology, Hasheminejad Kidney Center (HKC), Iran University of Medical Sciences, Tehran, Iran
5Department of Radiology, Shiraz University of Medical Sciences, Shiraz, Iran
*Corresponding author: Saeid Esmaeilian, Department of Radiology, Namazi Hospital, Shiraz University of Medical Sciences, Shiraz, Iran, Tel: +98 9120463698, E-mail: [email protected]
Received: December 31, 2022 Published: January 12, 2023
Citation: Esmaeilian S, et al. © (2023). Post Laparoscopic Myomectomy Gossypiboma with Cecum and Appendix Invasion: Case Report. Surgeries. 4(1):09.
Copyright: Esmaeilian S, et al. © (2023).
ABSTRACT
Introduction: Gossypiboma described retained surgical sponge in patient’s body after operations. That is a rare complication in laparoscopic surgeries, and due to vague and nonspecific clinical manifestations and also secondary complications such as perforation, fistula, and abscess formation. In this case report we describe a Gossypiboma after laparoscopic myomectomy with presentation of ambiguous pain and invasion into the cecum and appendix. So, it should be considered in susceptible patients even in laparoscopic surgeries. Case presentation: a 42-year-old woman with history of recent laparoscopic myomectomy and ambiguous pelvic pain from 3 months later. Imaging shows evidence of Gossypiboma. During the explorative laparotomy there was evidence of invasion of the cecum and appendix. And segmental resection had been done for patient. Patient with good condition had been discharged. Conclusion: Gossypiboma should be in the differential diagnosis of every post-surgery patient even in laparoscopic procedures.
Keywords: Gossypiboma, laparoscopy, myomectomy, surgery.
INTRODUCTION
Gossypiboma is common medical term for description of retained surgical sponge or cotton material in patient’s cavity after surgery [1]. Clinical presentation depends on location, size, pathophysiologic reaction, and adjacent organs. There is wide spectrum from incidentally finding (asymptomatic) to fibrous aseptic reaction symptoms such as abdominal pain, palpable mass, anorexia vomiting, weight loss, malabsorption, and even more complications such as obstruction, perforation, fistula, and abscess formation [2- 4]. Diagnosis of Gossypiboma is challenging issue between radiologists, Surgeons, and Emergency physicians due to its nonspecific clinical sign and symptoms and even radiologic manifestations. Due to mention reasons, Gossypiboma should be considered in differential diagnosis of any patient with previous history of surgical process with any complaint [1&5]. Remaining any foreign body after surgery is considered as Ubiquitous medical error. Gossypiboma is more common in the Laparotomy procedures rather than Laparoscopy process [6] there are rare cases that report Gossypiboma after laparoscopy. Here we report a case of abdominal Gossypiboma after laparoscopy with a history of passing sponge form material with her defecation.
CASE PRESENTATION
A 42-year-old woman was admitted in surgical unit with chief compliant of chronic abdominal pain from the 3 months ago that had intensified in recent days without any other associated complaint such as nausea or vomiting and lose weight. Patient at time of examination had no gynecological complaint and she had mentioned recent excretion of sponge like material during defecation. The only positive point in past medical history was a laparoscopic myomectomy 4 month ago. The patient had normal vital sign and only positive finding in physical exam was mild to moderate tenderness in right lower quadrant and supra-pubic area. No definite mass had been detected on palpation. In addition, Blood test results were unremarkable. CBC data only showed mild leukocytosis (WBC=11000).
Due to chronic abdominal pain CT scan had been requested by surgical team. Contrast-enhanced abdominal CT scan images showed mass like structure with calcified fibers in the mid line of lower abdomen at scout view and also no definite sign of free air in the scout view is noted. In the axial sequences there was well defined, thick wall, cysticsolid structure (mm) that contained air bubbles and some radio-opaque tortuous coarse fibers with no enhancement which located in the midline adjacent to the terminal ileum and cecum. In addition, there were some stranding around mention structure also adjacent bowel loops shows some degree of wall thickening. No sign of malignant Lymphadenopathy was detected although some reactive non-significant mesenteric Lymphadenopathy around structure. Other abdominal and pelvic organs such as uterus and both ovaries are remarkable.
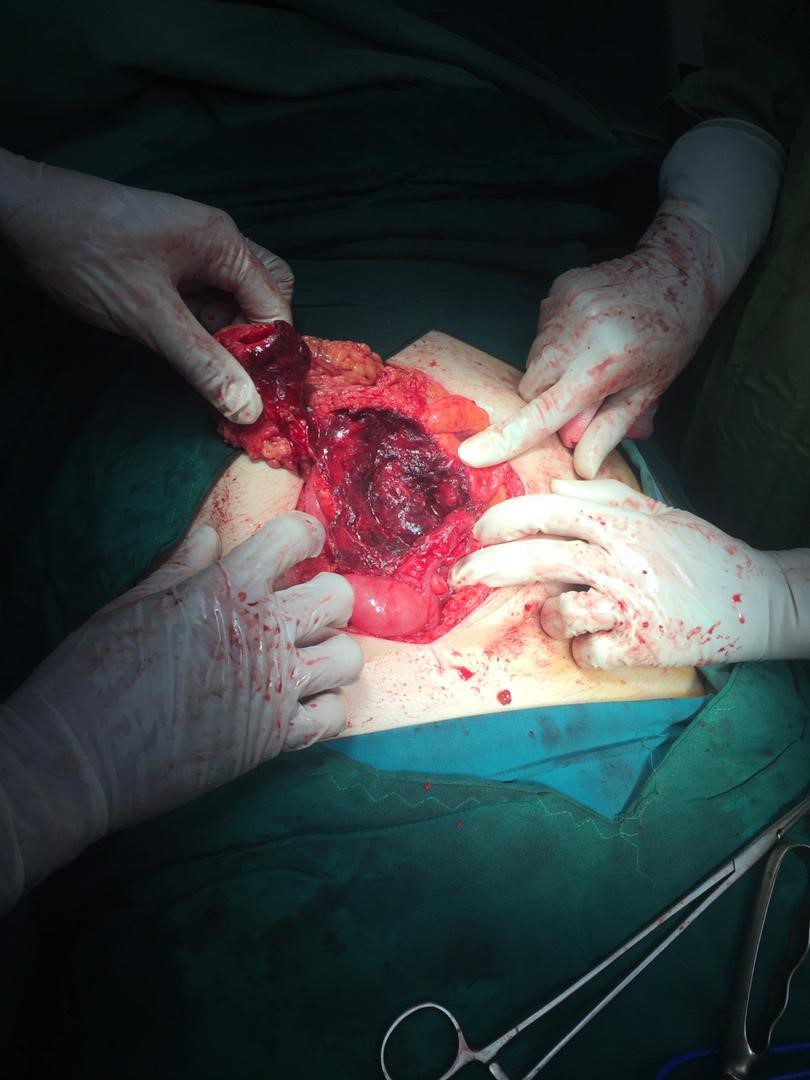
After imaging, Patient underwent laparotomy and surgical exploration discovered tense encapsulated lesion with notable adhesion to the adjacent bowels. Mention lesion had degree of invasion into the cecum and appendix wall. The Gossypiboma was resected (figure 5) and because of cecum and the appendix wall invasion, segmental resection and end to end anastomosis was done. No post-operative complications have occurred. Finally, after 4 days the patient discharged with good general condition. At 1-month follow-up, the patient had no other more symptoms.
Figure 5: Intra operative picture shows retained sponge
Pathologic examination showed that fibrotic tissue around foreign body (long gauze), and contained a purulent aseptic liquid with no malign cells.
Figure 1: Soft tissue opacity lesion with curved and banded radio-opaque lines suggestive for gossypiboma
Figure 2: Axial and coronal images show thick wall cystic lesion with entrapped gas bubble and hyperdense linear structure (spongiform appearance) compatible with Gossypiboma, also this lesion has close contact with cecum.
Figure 3: Encapsulated lesion with tense adhesion to surrounding bowels and perforated cecum.
Despite of development of surgical technics and strict protocols in the operation rooms, the remaining of foreign body is still is big challenge for surgeons. In Modern surgery, Gossypiboma is not accepted by any surgeon although it’s occurred between 1 in 800 to 18,000 abdominal surgeries [7] other authors believe that Gossypiboma incidence is under reporting and they estimated to be about 1 in 1000 to 1500 abdominal surgeries [1]. These differences show us this problem is a remarkable condition that needs to train more and revised surgical patient safety protocols.
The frequencies are more common in the open cavities such as the abdomen and the thorax (the most frequent sites) it has been reported in central nervous system, breast, bladder and extremities too [5&9].
In addition, laparotomy is more frequent surgical technic which associated with Gossypiboma. Almost no case report about Gossypiboma after laparotomy.
The most important mentioned risk factors for Gossypiboma are emergency operation, more than one surgical team, unplanned change in operation, change in nursing staff, inexperienced staff, long operation, volume of blood loss, surgical counts, high body mass index and female sex [2,6].
Some literatures believe that emergency operation, unexpected change in surgery and high body mass index are most impressive risk factors especially emergency operation [2]. And some other report gynecologic surgery in obese female as most probable situation for Gossypiboma [10] which is the same in our presented case.
Some literatures believe that emergency operation, unexpected change in surgery and high body mass index are most impressive risk factors especially emergency operation [2]. And some other report gynecologic surgery in obese female as most probable situation for Gossypiboma [10] which is the same in our presented case.
Its clinical manifestations depend on retained sponge size, location and also type of pathophysiologic reaction and vary from asymptomatic incidentally finding in patient with fibrous aseptic reaction to patients with abdominal pain, palpable mass, anorexia vomiting, weight loss, mal absorption, and more severe complications such as obstruction, perforation, fistula and abscess formation [1- 4] like our presented case that was complicated with cecum and appendix.
Diagnosis of Gossypiboma is challenging issue between radiologists, Surgeons, Emergency physicians due to the of its nonspecific clinical sign and symptoms and even radiologic manifestations. Due to mention reasons, Gossypiboma should be considered in differential diagnosis any patient with previous history of surgical process with any complaint [1,5]. CT scan is choice modality for diagnosis of Gossypiboma and also discrimination it from its possible differential diagnosis like abscess, hematoma, fecaloma, lymphocele, and neoplasm [1&11].
Other imaging modalities such as X-ray, Ultrasound or even MRI appearances are nonspecific or even can be confusing. So that CT scan had preferred for diagnosis of Gossypiboma rather than other modalities although when patient presented with ambiguous symptoms other modalities shows some similar appearance like that are describe in the CT scan. The most characteristic appearance is “spongiform pattern”, entrapped gas bubble cystic lesion with hyperdense linear structures [9&10]. Other suggestive feature for Gossypiboma is “whorl-like appearance”, opacified area with gas bubbles [9].
The most important point in Gossypiboma is that clinicians should consider it as a differential diagnosis in any patient with abdominal pain or any other nonspecific manifestations after any surgical procedures to prevent its morbid complications by opportune diagnosis.
CONCLUSION
Gossypiboma is a rare complication of surgical procedures with unspecific manifestations which can lead to serious complications. So, Gossypiboma should be in the differential diagnosis of every post-surgery patient even in laparoscopic procedures.
CONFLICTS OF INTEREST
All authors have no conflicts of interest.
SOURCES OF FUNDING FOR RESEARCH
No funding has been used for this research.
ETHICAL APPROVAL
Bushehr ethical committee of Bushehr University of Medical Sciences and ethical code 1400-451 had been given.
INFORMED CONSENT
Patient had read and understands the provided information and had had the opportunity to ask questions. And privacy of patient had been guaranteed. Patient gave a copy of informed consent form.
REFERENCES
1. Srivastava KN, Agarwal A. (2014). Gossypiboma posing as a diagnostic dilemma: a case report and review of the literature. Case Rep Surg. 713428.
2. Aminian A. (2008) Gossypiboma: a case report. Cases Journal. 1(1):220.
3. Eken H, Soyturk M, Balci G, Firat D, Cimen O, Karakose O, et al. (2016). Gossypiboma mimicking a mesenchymal tumor: a report of a rare case. Am J Case Rep. 17:27-30.
4. Lata I, Kapoor D, Sahu S. (2011). Gossypiboma, a rare cause of acute abdomen: A case report and review of literature. Int J Crit Illn Inj Sci. 1(2):157-160.
5. Kori R, Bains L, Jain SK. (2019). Intravesical gossypiboma: our experience and the need for stringent checklist and training. BMJ Case Rep. 12(2):e227278.
6. Meenakshi G, Mahaveer R, Surekha B, Pratibha S, Garima Y, Priyanka S. (2019). Gossypiboma – A Nightmare for Surgeon: A Rare Case with Review of Literature. J Midlife Health. 10(3):160-162.
7. Gawande AA, Fisher ES, Gruber J, Rosenthal MB. (2009). The cost of health care—highlights from a discussion about economics and reform. N Engl J Med. 361(15):1421-1423.
8. Stephany VM, Marialy DG, Bianco TC, Mora EH, Rojas RR, Malave YC, et al. (2015). Duodenal gossypiboma: a case report and literature review. Invest Clin. 56(3): 296-300.
9. Kabba MS, Forde MY, Beckley KS, Johnny B, JahKabba AM, Seisay SB, et al. (2020). Gossypiboma with perforation of the umbilicus mimicking a complicated urachal cyst: a case report. BMC Surg. 20(1):242.
10. Mathew RP, Thomas B, Basti RS, Suresh HB. (2017). Gossypibomas, a surgeon’s nightmare—patient demographics, risk factors, imaging and how we can prevent it. Br J Radiol. 90(1070):20160761.
11. Batra R, Gautam R, Manchanda A, Ghuliani D. (2021). A Case of Two Abdominal Gossypibomas in a Patient: A Rare Case Report. Journal of Gastrointestinal and Abdominal Radiology. 04(02):161-165.
 Abstract
Abstract  PDF
PDF.jpg)

.JPG)